Background: Disparities in survival between adolescents and young adults (AYA) treated for acute lymphoblastic leukemia in pediatric versus adult centers are well documented. Whether similar disparities exist among AYA with mature B-cell non-Hodgkin lymphoma (B-NHL) is unknown, despite substantial differences between pediatric and adult treatment protocols. We compared outcomes among AYA with B-NHL by locus of care (LOC; pediatric versus adult) using a population-based clinical AYA database. We also assessed whether socioeconomic status or geographic area impacted outcome in this population.
Methods: The IMPACT cohort comprises all Ontario, Canada AYA aged 15-21 years diagnosed with one of six common cancers (including NHL) between 1992-2012. Detailed demographic, disease (histology, stage), treatment, and outcome data were collected through chart abstraction and validated by content experts. Postal code at diagnosis allowed determination of neighbourhood income quintile and rural residence. Linkage to population-based health administrative data identified additional events (second cancers, relapse, death). Event-free (EFS) and overall survival (OS) were determined using Kaplan-Meier methods. The impact of LOC on EFS and OS was determined using multivariable Cox proportional hazard models, adjusted for demographics and disease-related variables.
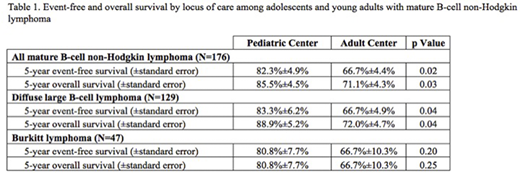
Results: Among 176 AYA with B-NHL, 62 (35.2%) received therapy at a pediatric center. Pediatric center AYA were more likely to have Burkitt lymphoma (BL) than diffuse large B-cell lymphoma (DLBCL) as compared to adult center AYA [26/62 (41.9%) vs. 21/114 (18.4%); p<0.001], and more likely to have advanced stage (i.e. Stage III/IV) disease [38/62 (61.3%) vs. 46/114 (40.4%); p=0.006]. The 5-year EFS and OS (with standard errors) for the whole cohort were 72.2%±3.4% and 76.1%±3.2%. Both EFS and OS were superior among pediatric center patients (EFS 82.2%±4.9% vs. 66.7%±4.4%; p=0.02), (OS 85.5%±4.5% vs. 71.1%±4.3%; p=0.03). When stratified by histology (BL vs. DLBCL), the EFS and OS were similar. However, the superior outcome of pediatric center AYA retained statistical significance only among those with DLBCL (Table 1). Adjusted for histology (BL vs. DLBCL), stage, and time period of diagnosis, adult center AYA had inferior EFS [hazard ratio (HR) 2.4, 95% confidence interval (95CI) 1.1-4.9, p=0.02] and OS (HR 2.5, CI 1.1-5.7, p=0.03). Neither neighbourhood income quintile nor rural residence was associated with EFS or OS.
Conclusions: In this population-based cohort, AYA with B-NHL treated at pediatric centers experienced substantially superior EFS and OS compared to those treated at adult centers, even accounting for disease characteristics. In subgroup analyses, this difference retained statistical significance among patients with DLBCL but not among patients with BL, though the latter analyses were limited by small sample sizes. Future analyses will analyze whether patterns of treatment failure and late effects vary by locus of care. Further confirmatory studies are warranted, as are studies to determine the relative contribution of pediatric protocols versus other components of care. Our results nonetheless suggest that similar to AYA with acute lymphoblastic leukemia, AYA with B-NHL may benefit from being treated in pediatric centers with pediatric protocols.
Baxter:Servier: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal